Surgery for Low Back Pain
Low back pain is the TOP cause of disability, WORLDWIDE, and it’s a condition that every Physiotherapist has come across at some point in their career.
Even though medical technology is advancing, the incidence of Low Back Pain is not decreasing, and in fact, continues to increase year on year.
For people who suffer an acute episode of severe low back pain, I’m sure the possibility of the need for surgery has crossed their mind at least once.
But is Surgery always indicated?
The answer is NO.
THE GOOD NEWS
Up to 90% of Low Back Pain and their related symptoms (eg, Sciatica) can, and should be treated CONSERVATIVELY first.
Conservative treatment options commonly include Physiotherapy, Chiropractic, Osteopathy and Self Management Strategies.
If managed properly through conservative measures, most low back pain occurrences will subside.
And for even longer term results, a thorough assessment into the unique contributing factors to the development of a person's low back pain should be conducted, so bespoke exercises can be prescribed for long term spinal health.
At Physiologic, we’re experts in the treatment and long term solutions for Low Back Pain. Our sessions will always include an individualised program aimed at addressing your weak links, to ensure long term results. Contact Us to talk with our Physiotherapist about how we can help with your Low Back injury.
THE BAD NEWS
Unfortunately, there are some less common cases where surgery is definitely indicated, as there is an immediate risk of long term damage or poor prognosis with conservative treatment.
We will briefly look at some causes of low back pain that will require prompt surgical intervention.
CONDITIONS REQUIRING SURGERY
1: Cauda Equina
This condition describes excruciating low back pain and leg pain, associated loss of sensation in the saddle area, and loss of bowel and bladder control and weakness in the legs.
It’s usually caused by a massive disc herniation, but can also be caused by severe degenerative changes, direct trauma, spinal tumours or even birth abnormalities.
Surgery is indicated promptly to ease the pressure off the nerve roots, and to restore function to the organs and lower limb muscles.
Over the course of a Physiotherapists’ career, they may only come across ONE case of Cauda Equina.
2: Massive Disc Herniation causing motor and sensation loss
When somebody experiences a massive disc herniation, they commonly present with lots of shooting leg pain, making it difficult to sit, and find a comfortable position to sleep.
Motor loss is evident with a weakness in the calves, toes, glutes and hamstrings. Sensation loss presents as numbness and loss of ‘proprioception’ in the feet commonly.
These people may not immediately go for surgery, as their Spinal Specialist may sometimes trial a period of conservative treatment - usually Specialist Physiotherapy, to see if their symptoms will resolve in around 4-6 weeks time.
If there is no improvement, or if the condition worsens, Spinal Surgery may be indicated to minimise nerve damage and muscle atrophy.
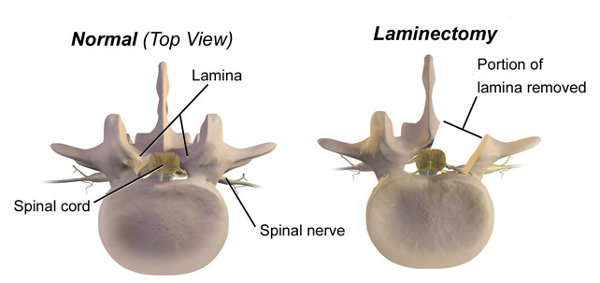
Common procedures include a discectomy (removing herniated disc material), Laminectomy (shaving off some bone to reduce the pressure in the spinal canal), or a combination of both coupled with some sort of Spinal Fusion.
3: True Spinal Instability (Unstable Spondylolisthesis)
Usually in the older population group, a true unstable spondylolisthesis may be required to be operated on, IF, the client is symptomatic, and is at risk of developing ‘hard neurological signs’, including loss of motor function and sensation loss.
The decision making process is usually multi disciplinary, meaning the Spinal Specialist will discuss the clinical and radiological findings with the Specialist Physiotherapist, to determine if the client will likely benefit from the surgery, and whether or not they are likely to be able to rehabilitate successfully post surgery as well.
POST SPINAL SURGERY PHYSIOTHERAPY REHABILITATION
Spinal surgeries are generally complex procedures, and it is common for people to have a temporary period of increased pain post surgery, as the inflammation around the surgical site will likely have an irritating effect on the nerves.
To reduce your pain as soon as possible, and regain your physical function, we highly recommend working with a Physiotherapist experienced in Spinal post operative care. Not all Physiotherapists have a good understanding of certain spinal operations and their specific nuances, and selecting a Physiotherapist who has a good relationship with the operating surgeon is always the preferred choice.
Physiotherapy rehabilitation will focus primarily on helping you
1: Reduce your pain
2: Regain your mobility safely
3: Regain you muscular strength and function
4: Get you back to your daily activities/sport/exercise
5: Injury prevention.
Don’t leave your Post Operative care to chance, our Physiotherapist has extensive experience in the careful rehabilitation of clients post Spinal Surgery, and has excellent relationships with some of Hong Kong’s Top Spinal Surgeons.
If you’ve just had Spinal Surgery, or unsure if surgery is indicated for you, click below to request a call back from our Spinal Physiotherapist for a no-obligation chat about how we can help.
ABOUT THE AUTHOR
Ryan Tan is our Clinical Director and Physiotherapist here at Physiologic Hong Kong. He’s had over 10 years of experience as a sports and spinal Physiotherapist. He has acquired his Certificate of Spinal Manual Therapy (COSMT), which is an intensive course focussing purely on treating spinal conditions. He has extensive experience working in Complex Pain Clinics in London, treating complex spinal conditions that have been through Spinal Surgeries and procedures. Ryan now works closely with Orthopaedic Spinal Specialists to provide collaborative care and expert Physiotherapy treatment to those suffering from back pain. If you have a complex Spinal injury that hasn’t been able to be resolved, contact us for a no obligation assessment!