What you need to know about Tendon Injuries (Tendinitis or Tendinopathy)
Tendon injuries are a difficult presentation for many Physiotherapists to treat due to their volatile nature, and lengthy recovery times.
Treatment and rehabilitation protocols demand precision to create an optimal healing environment, and that takes exceptional physiotherapy clinical skills and experience in treating tendon injuries.
We’ve had countless athletes walk through our doors feeling deflated about their tendon injury plateauing, unsure if they’ll ever return to their sport. With an accurate diagnosis, evidence based treatment principles and your persistence, most tendon injuries do recover!
If you’re in a similar position, we’ll outline the most important things you need to know about tendon injuries, giving you insights into how best to manage it.
Over the next few blog posts, we’ll also take a deeper dive into the specifics of particular tendinopathies.
WHAT IS A TENDON?
A tendon is a ‘connective soft tissue’ structure in your body, that is packed full of Type 1 Collagen fibres that are aligned parallel to each other, creating a strong, robust structure.
The collagen fibres are separated into bundles, and the bundles are also connected strongly to each other, with some blood vessels in between them.
The tendon gets stronger when you gradually load it (exercise).
And conversely, will weaken if you are inactive for 1-3 weeks.
Tendon strength increases by packing even more collagen into the bundles, strengthening the bonds between each collagen fibre, and ensuring a parallel formation is maintained.
WHAT IS THE FUNCTION OF A TENDON?
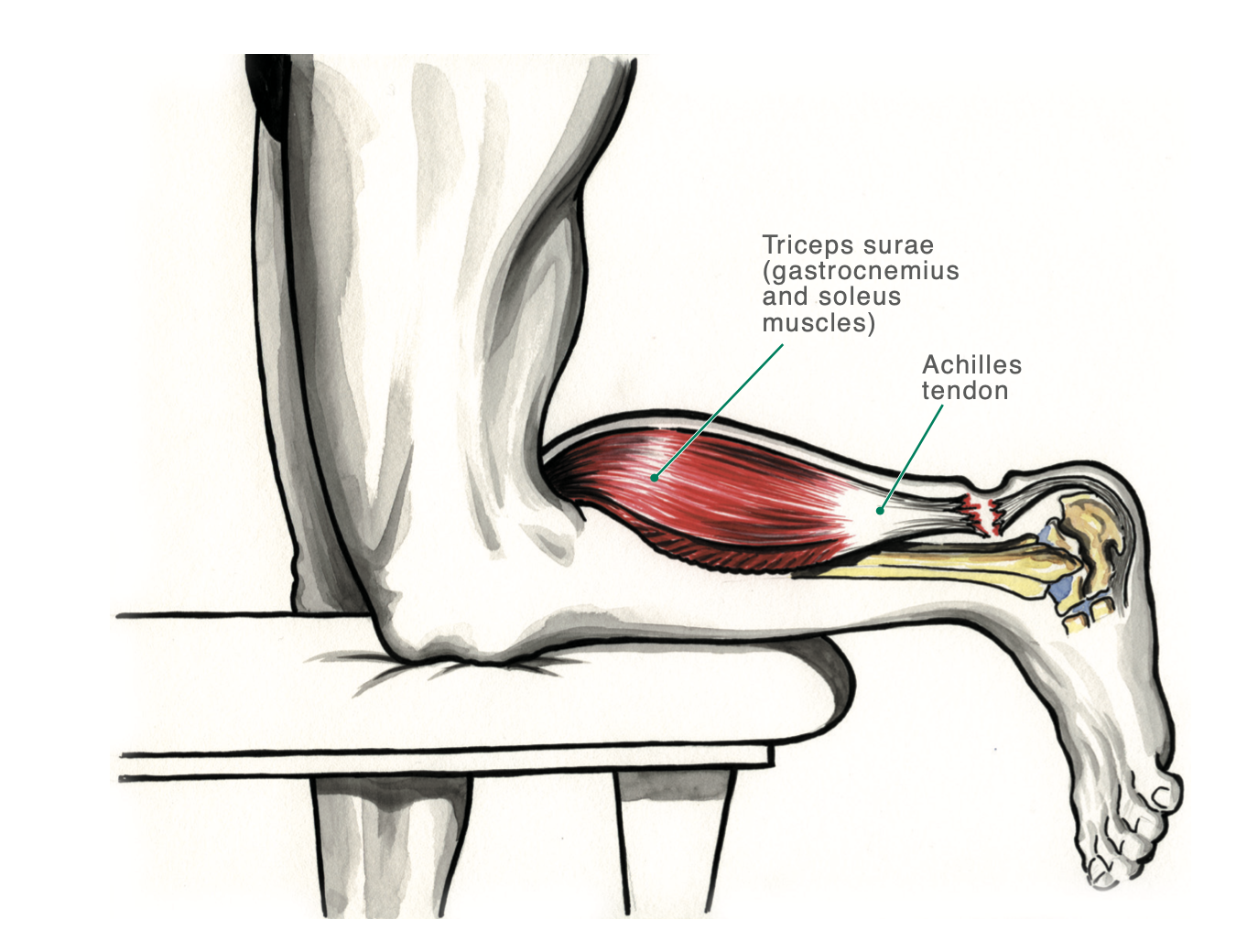
In a nutshell, a Tendon connects BONE to MUSCLE. (Ligaments connect bone to bone).
This means that when a muscle contracts, its force is being transferred through the Tendon, over to the bone.
That force can result in
Movement (eg: running, walking, swimming)
Deceleration and load absorption (eg: landing after you’ve jumped)
Holding a still position (eg: doing a roman chair)
One of the unique properties of a tendon is its ELASTICITY.
It has a unique ability to absorb force as it lengthens, and rapidly convert that into movement as it shortens, very much like a rubber band.
The effects of its elasticity is seen in dynamic sports like running, basketball and volleyball, where explosive movements are common.
TENDINITIS OR TENDINOPATHY?
When it comes to the proper terminology for tendon injuries, Physiotherapists and other health professionals up to date with the latest research prefer to use TENDINOPATHY.
‘Pathy’ relating to ‘problem’, or ‘pathology’.
Tendinopathy = problem of the tendon.
The reason we don’t use Tendinitis anymore, is that research has proven that there is no significant signs of inflammation in the tendon during these injuries.
So using the term tendinitis (‘itis’ relating to inflammation) is inaccurate.
CAUSES OF TENDON INJURY
Now that we know the primary function of the Tendon is to transfer force from muscles to bones, it leads to the question - what is the most common cause of a tendon injury?
In our experience - Excessive force that exceeds the tendons capacity.
The term ‘excessive force’ is an umbrella term that we use to describe different ‘parameters’ of force that could happen. Let’s take a look at some common scenarios.
1: Acute Overload of a Tendon
A common mechanism that Physiotherapists encounter, this describes a sudden increase in exercise that the tendon is unaccustomed to.
For example, a client who’s never run before, decides to go on a health kick and runs every day 5 days straight.
Their Achilles or Patellar tendons are likely to get injured as they were unaccustomed to regular running, and their collagen fibres could not tolerate the daily running load.
As a result, it swells up, disorganises the parallel formation of the tendon, and causes pain in the knee.
Other common examples include Jumpers Knee (Patellar tendinopathy), or Rotator cuff Tendinopathy.
2: Gradual Overload of a Tendon
This particular mechanism is more applicable to people who perform repetitive tasks, like swimmers, runners, or even tradesmen like electricians and plumbers.
Take a swimmer for example. Swimming multiple laps of freestyle requires repetitive use of the same shoulder muscles (rotator cuff).
If their rotator cuff muscles are not in good enough condition (Strength, Endurance and Mobility), there is a chance that the tendons will eventually be overloaded, causing a breakdown of the parallel formation of the collagen fibres, resulting in pain.
In this Gradual Overloading mechanism, we’ve found that it is crucial to look at the requirements of the sport as a whole, and uncover the reasons WHY the tendon was overloaded.
It is common for us to find a breakdown in the kinetic chain somewhere else distant from the shoulder that has resulted in a gradual tendon overload.
Taking the swimmer as an example again, if their thoracic spine does not have the flexibility into rotation and extension, the rotator cuff muscles have to work extra hard to lift the shoulder even higher at every single stroke to clear the water.
Other common examples include Achilles and Hamstring tendinopathies.
3: A sudden large force exceeding the Tendon's structural capacity
This mechanism describes a sudden, large force that is imposed on a tendon (that is usually deconditioned already), resulting in a rupture.
Commonly, we see this in the Achilles Tendon when someone is pushing off to sprint, or has just landed from a jump and was intending to push off into a different direction (basketball).
A significant risk factor is a poorly conditioned tendon, and weak muscles that attach into the tendon.
BASIC PRINCIPLES TO PREVENT & REHABILITATE TENDINOPATHIES
GRADUAL PROGRESSION OF LOADING
Probably the most important factor in tendon injuries, it is crucial to ensure that you are paying close attention to load management.
Going too hard too soon is a sure way to set yourself up with an acute tendon injury.
If you’re getting back into running after not having done it for a while, start off conservatively to minimise your risk of injury, by allowing your tendons to adapt to running.
For example, you could start running 2-3 days/week, with at least 2 days rest in between. After a period of 2-3 weeks, you could progress by either increasing the distance, or speed at which you run.
SLOW & CONTROLLED STRENGTHENING
If you’re going through a tendinopathy now, you should be doing some kind of rehabilitation exercises prescribed by your Physiotherapist.
It’s important to perform them slowly and under control, as this is what stimulates your body to lay down and strengthen those Type 1 Collagen fibres in your tendon.
ISOMETRICS FOR PAIN RELIEF
Performing heavy isometrics for the tendon have proven to have an analgesic effect (pain relief) for tendons.
This is an added benefit alongside increasing its capacity, stiffness, and muscular strength.
Spanish Squats, Isometric exercise for Patellar Tendinopathy
FUNCTIONAL CHAIN STRENGTHENING/MOBILITY
FUNCTIONAL CHAIN STRENGTHENING/MOBILITY
Rehabilitating tendon injuries isn’t just about the tendon.
With a thorough assessment of your body, your Physiotherapist should be able to determine contributing impairments that have led to the development of your tendinopathy.
It’s not uncommon for our team at Physiologic to prescribe glute and core work for a Rotator Cuff tendinopathy in a tennis athlete.
At Physiologic, we look at your body as a whole, in relation to the sport you play. Addressing certain deficits is key for long term solutions, injury prevention and longevity for your game.
COMPLETE REST IS NOT HELPFUL
As tendons will respond to load that is imposed on them (addition or removal of load), it is rarely (if ever) advisable to completely rest.
Completely resting will further weaken the tendon, as the body thinks that it’s not doing exercise anymore, so it is not encouraged to strengthen the injured tendon.
SHOCKWAVE THERAPY
For chronic, or calcific tendinopathies, there is a growing and emerging number of studies that support the use of Shockwave to promote recovery.
At Physiologic, we have a premium PiezoWave 2 Shockwave machine that our Physiotherapists use regularly for the successful treatment of chronic tendinopathies.
Contact us for more information on how we use shockwave as part of our Physiotherapy programs to help.
CONCLUSION
The key for the successful treatment of tendinopathies is finding the right balance and recipe of rehabilitative exercises to do that relieves pain, improves the structural integrity of the tendon, and gets people back to their chosen sport.
If you’ve been dealing with a tendinopathy that is stopping you from getting back to the things you love, contact us here to see how we can work with you through the rehabilitation process.
Stay tuned for our following blog posts as we’ll take a deeper dive into specific tendinopathies, sharing some clinical pearls along the way.
About the Author
Ryan Tan is our Clinical Director and Physiotherapist here at Physiologic Hong Kong. He’s had over 10 years of experience as a sports and musculoskeletal Physiotherapist, having looked after elite athletes such as the NZ Rugby 7’s team and more recently, some of Hong Kong’s top Trail Runners. He attributes his clients successes to their commitment in being diligent with their individual rehabilitation programs, and curated treatment protocols for each individual. Excellent relationships with some of Hong Kong’s top Orthopaedic Surgeons also allows Ryan to provide a truly multidisciplinary team approach to his client’s health care. Contact us to speak with Ryan if you are looking for an experienced Physiotherapist to guide you back to your competitive best!